ApoB and Lp(a): The Silent Cholesterol Risks You Can’t Ignore
What are ApoB and Lp(a)?
Apolipoprotein B (ApoB) is the protein found on every atherogenic lipoprotein particle (one ApoB per LDL, VLDL, IDL and Lp(a) particle). Measuring apoB gives a direct count of circulating atherogenic particles — which often predicts risk better than LDL-C (cholesterol mass). In other words, apoB tells you the number of “bad” particles, not just how much cholesterol they carry. (Circulation review on apoB)
Lipoprotein(a) — Lp(a) is an LDL-like particle linked to an additional protein called apolipoprotein(a). Lp(a) is largely genetically determined, stable across life, and confers both pro-atherogenic and pro-thrombotic risk — meaning it raises the chance of plaque and of clotting events like heart attack and stroke independent of LDL-C. (NLA focused update on Lp(a), 2024)
How are they different from LDL?
LDL-C measures cholesterol mass inside LDL particles. Two people can have identical LDL-C but very different particle counts — one with fewer, cholesterol-rich particles and one with many small particles. ApoB measures particle number directly; where apoB and LDL-C disagree (discordance), risk generally follows apoB. Lp(a) is a separate, genetically driven particle that adds risk beyond LDL or apoB. (Standardization and evidence for apoB)
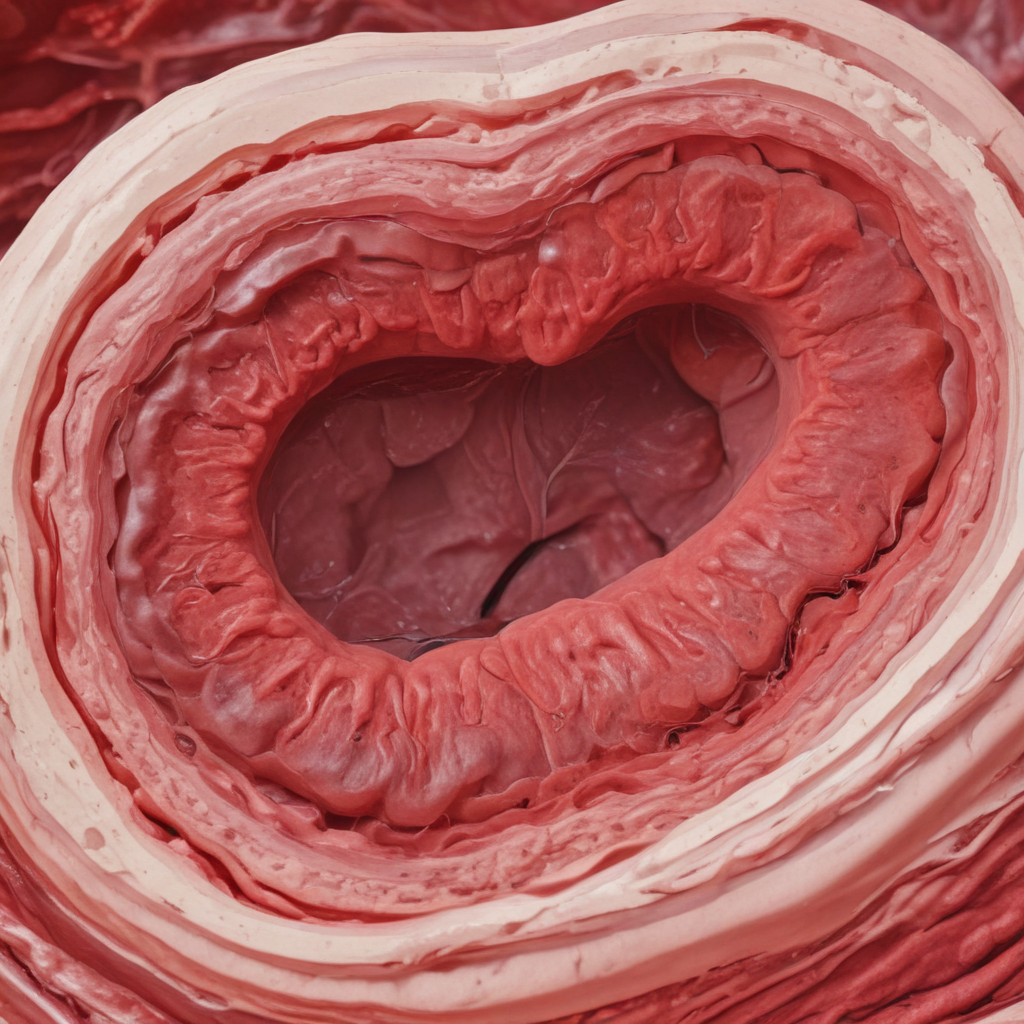
Why are elevated ApoB and Lp(a) dangerous?
More atherogenic particles (high apoB) mean greater lifetime exposure of vessel walls to cholesterol-rich particles — the fundamental driver of atherosclerosis. Elevated Lp(a) accelerates plaque formation and increases thrombosis risk through its apolipoprotein(a) component; high Lp(a) is also linked to calcific aortic valve disease. These mechanisms explain why individuals can still have events despite “normal” LDL-C. (Review: Lipoprotein(a) updates)
Who should be tested? — NLA’s focused update (2024)
The National Lipid Association’s 2024 focused update recommends measuring Lp(a) at least once in adulthood to identify elevated levels and guide risk stratification; cascade testing of first-degree relatives is advised when Lp(a) is high. The update provides practical thresholds (approximate conversions): <75 nmol/L (~30 mg/dL) = low risk; 75–125 nmol/L (~30–50 mg/dL) = intermediate; and ≥125 nmol/L (~50 mg/dL) = high risk, though labs report in mg/dL or nmol/L — know which unit your lab uses. (NLA focused update (PDF))
ApoB is particularly helpful when LDL-C is discordant with clinical picture — for example, in diabetes, metabolic syndrome, obesity, high triglycerides, or chronic kidney disease. Several expert statements and consensus documents now recommend using apoB (or non-HDL-C) to refine risk and treatment targets. (ApoB: Bridging evidence & practice)
Is there a treatment? Are statins useful?
Yes. Lowering the number of atherogenic particles reduces events. Statins remain the first-line therapy: they reduce LDL-C and lower apoB (particle number) and clearly reduce cardiovascular events. When additional lowering is needed, add ezetimibe and then PCSK9 inhibitors — these further lower LDL-C and apoB. (Circulation apoB review)
For Lp(a), traditional drugs have limited effects: statins have little consistent lowering of Lp(a) and sometimes modestly increase it; PCSK9 monoclonal antibodies reduce Lp(a) by roughly 20–30% in trials, likely via effects on particle clearance. Crucially, targeted Lp(a) therapies are now in advanced development — antisense oligonucleotides and small interfering RNA (siRNA) agents (pelacarsen, olpasiran, lepodisiran and others) dramatically reduce Lp(a) levels (some agents >80–90% in phase 2) and large outcome trials (HORIZON, OCEAN(a), ALPACA and others) are ongoing to determine whether lowering Lp(a) reduces events. (HORIZON (pelacarsen), OCEAN(a) (olpasiran), ALPACA (lepodisiran); see also recent reviews).
Impact of lifestyle and alcohol
Healthy lifestyle — Mediterranean-style diet, regular exercise, weight loss when needed, smoking cessation, blood-pressure control — lowers overall cardiovascular risk and reduces apoB-rich triglyceride particles. However, Lp(a) is largely genetically determined and is usually unchanged by diet or exercise; lifestyle remains essential to lower the non-Lp(a) components of risk. Alcohol does not meaningfully lower apoB or Lp(a) and heavy consumption worsens overall cardiovascular risk — so alcohol is not a treatment strategy for lipids. (Cleveland Clinic: ApoB test)
How to act on a high results
- If ApoB is elevated: intensify LDL-lowering therapy (statin → ezetimibe → PCSK9 inhibitor) to lower particle number and event risk.
- If Lp(a) is high: aggressively treat modifiable risks (LDL-C, blood pressure, smoking), consider family screening, and discuss eligibility for clinical trials of Lp(a)-lowering agents as they become available.
- Document Lp(a) once (per NLA) and place the value in the medical record for future reference; cascade test first-degree relatives if elevated.
Bottom line
ApoB and Lp(a) reveal cardiovascular risk that routine LDL-C can miss. The 2024 NLA focused update raises testing of Lp(a) to routine practice (at least once in adulthood) and highlights the role of apoB for better risk discrimination. Statins and PCSK9 inhibitors reduce apoB and lower events; targeted Lp(a) drugs are promising and outcome trials are underway. Ask your clinician about testing for ApoB and Lp(a) if you have a family history of premature heart disease, unexplained high-risk features, or discordant lipid results.
Life in Balance MD is led by Dr. Amine Segueni, a board-certified physician dedicated to delivering clear, evidence-based health insights. His passion is helping readers separate facts from myths to make smarter, healthier choices. Content is for educational purposes only and not a substitute for medical advice.